The Foreign Aid Bridge Fund (FABF) is an emergency project by Panorama Global aimed at providing continuity support for lifesaving activities following the termination of the USAID KCHS Activity. FABF is a four-month project, running from 20th April 2025 to 20th August 2025. It is implemented in Masaka, Kalangala, Mpigi, Kalungu, Ssembabule, Bukomansimbi, and Masaka City, in collaboration with all health facilities—both public and private.
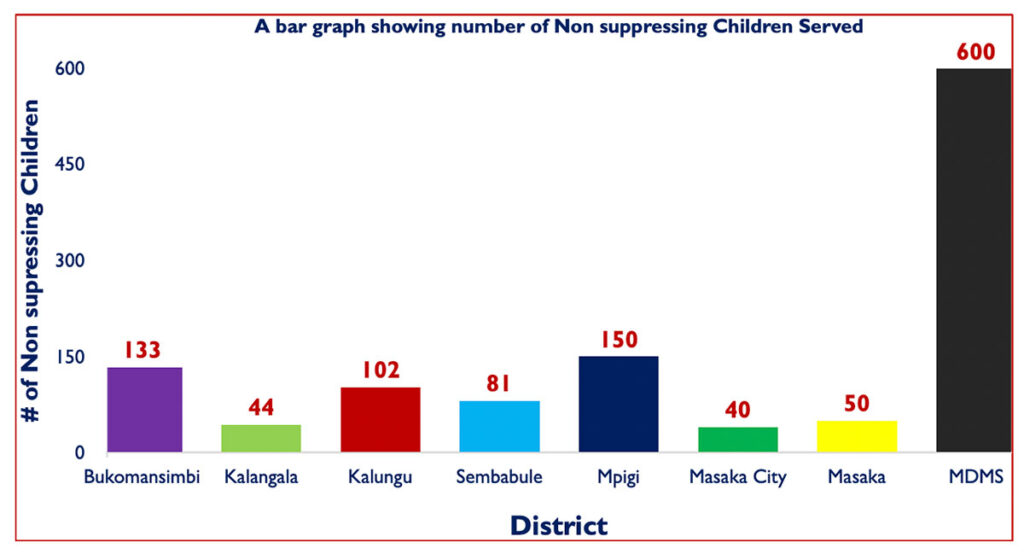
During the USAID-KCHS Activity implementation, MDMS reached 407 non-suppressing children (0–17 years). Through home visits for Intensive Adherence Counselling (IAC) sessions, the most common reasons for non-suppression among children included:
- Poor adherence (90%) due to uncommitted treatment supporters, poor time management, and improper drug storage.
- Pill burden, over- or under-optimization, insufficient food, and limited HIV knowledge—especially among HIV-negative caregivers.
To address these challenges, the MDMS team provided targeted services to both children and caregivers, including:
- ART literacy, disclosure and post-disclosure support, and mental health psychosocial support.
- ART refill appointment reminders, nutritional screening and education, TB screening, and HIV prevention and WASH messages.
Purpose:
To provide one-time emergency general operating support to sustain the continuity of previous OVC services.
Target:
Non-suppressing CLHIV (Children Living with HIV) are our primary beneficiaries. The project enrolls households with NS_CLHIV, including their siblings.
Achievements:
In May, 456 IAC sessions were conducted across all districts. While identifying root causes for non-suppression, caregivers, children, and the MDMS team collaboratively developed specific action plans to support adherence. These plans are implemented by treatment supporters and monitored by social workers.
One caregiver shared:
“We had become worried when we heard that America had stopped funding ARVs in Uganda—that’s why we broke the tablets to make them last longer. Now that Counsellor Sarah has explained and assured us that drugs are freely available at the facility, we are happy and ready to collect new drugs and take them as prescribed.”
To promote retention in care, 230 CLHIV were line-listed for appointments. Of these, 218 attended, while 12 missed due to reasons such as caregiver forgetfulness and lack of transport. These cases were tracked and followed up by para-social workers, who either conducted home drug deliveries or escorted the children to their healthcare facilities for ART refills.
Integrating mental health services into community IAC sessions has helped identify treatment barriers among CLHIV, enabling tailored services and treatment literacy.
Lessons Learned:
- Engaging health facilities during entry meetings and identification has strengthened collaboration, promoting joint home visits and action planning.
- Leveraging existing community structures, such as para-social workers, fosters community ownership and sustainability. Caregivers openly share challenges with trusted para-social workers.
- Integrating mental health services into IAC sessions has uncovered mental stressors contributing to poor adherence—especially among adolescents—allowing MDMS to provide targeted psychosocial support.
