The Safe Birth Project was born in 2016 when Bishop Kaggwa the Bishop of Masaka Diocese tasked Dr. Sherry Teefey, Professor of Radiology at Washington University, to address the challenge of obstetric fistula in Masaka, Uganda. Uganda has one of the highest obstetric fistula rates in the world. It is caused by obstructed labor and the only treatment is a cesarean section. Basically, during labor, the baby’s head gets stuck and crushes the pelvic tissues. The end result: if the mother does not die, she leaks urine and/or stool and is ostracized by her family and village.
In the rural districts, village health centers (VHCs) have skilled midwives, but only 44-53% of mothers are delivered by a skilled birth attendant. Why is this? There are many reasons including access to health care resources, lack of education, poverty and remote distance from healthcare facilities; barriers outlined by the World Health Organization (WHO) in 2019.
The “Safe Birth Project” uniquely brings together ultrasound, obstetric fistula education and microfinancing to address these challenges. After a year of planning, that included discussions with Mindray North America who partnered with us, the Safe Birth Project was launched in January of 2017. As of January 2023, there are portable ultrasound machines at 22 VHCs. Midwives were trained to diagnose three high-risk obstetric conditions that would mandate delivery at a medical facility with an obstetrician. – Abnormal fetal lie, placenta previa (obstruction of the birth canal by the placenta) and twins.
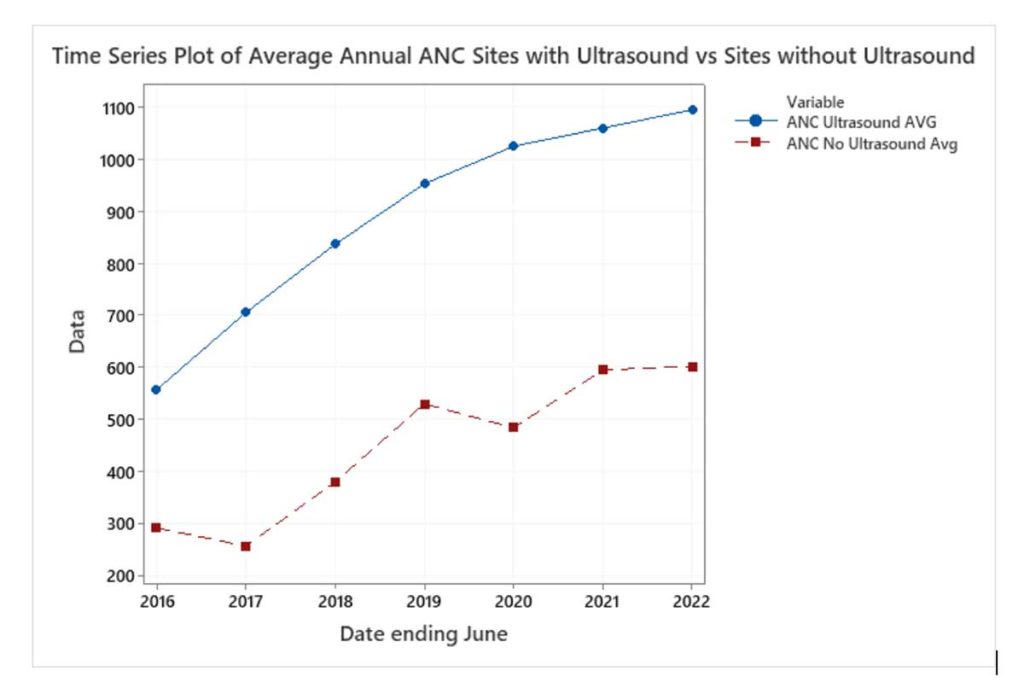
A midwife was also trained as a sonographer and now provides remedial training to the midwives in basic and advanced ultrasound and works with the midwives to educate mothers about the cause of obstetric fistula and importance of delivering at a VHC. Data shows that the program has been successful; the introduction of ultrasound has motivated mothers to come to the VHCs for antenatal care compared to VHCs without an ultrasound machine (graph 1). In fact, 11,335 ultrasounds were performed between July 2021 to June 2022 and 297 high risk conditions were diagnosed and appropriately managed or referred.
However, many of our mothers struggled to pay their fees – this is where microfinancing comes in. In 2018, Microfinancing was introduced to the VHCs and provided funds to develop microfinancing projects (piggeries, event or room rentals). Mothers were granted piglets (with an expectation of payback to the program) and trained in piggery management by our vet technician. Over time, the mothers realized profits and thus had the financial means to pay for their antenatal services and health care.
After a long hiatus due to COVID, we were able to return to Uganda in January 2023. It was evident that midwives had embraced ultrasound and it was now an integral part of antenatal care. We also visited mothers who had been granted a piglet and heard many success stories. We visited mothers who had begun second businesses such as animal husbandry (goats, chickens), or started coffee plantations or small retail businesses who could now pay for their health care, send their children to school and buy food for their families. Despite COVID, drought, famine and Ebola, the VHCs have persevered. We could not be happier!
A very special Thank You to Mindray North America; without their partnership and continuing support, this program would not exist.